Free shipping on purchases over $69
Nourishing the Mind-to-Be: Essential Nutrition for Fetal Brain Development
Written by: Marci Clow, MS, RDN
A nutrient-rich diet during pregnancy is crucial for providing the building blocks necessary for healthy fetal brain development. While adequate nutrition is critical throughout the gestational period, fetal brain development is particularly vulnerable to a lack of nutrition during the early stages of pregnancy. Research also indicates that nutrition in the prenatal environment has a significant effect on shaping neurocognitive development after birth. This article will dive into nutrients that contribute to nourishing a developing brain from conception to birth.
What Are the Key Nutrients for Fetal Brain Development?
During the dynamic state of pregnancy, the female body goes through many physiological changes to miraculously produce a new life. Consuming a wide variety of nutrient-rich foods throughout gestation can profoundly impact a healthy pregnancy and outcome. Although all nutrients are important, certain nutrients are particularly critical for the development and growth of the fetal brain during different stages of gestation.
Folate (Folic Acid): The Neural Tube Defender
Folic acid is the synthetic form of folate used in supplements and fortified foods. It is essential for brain and spinal cord formation and preventing neural tube defects (NTDs). The neural tube starts out as a tiny ribbon of embryonic tissue, and by the 28th day, it is beginning to form into a spinal cord. When folic acid is deficient, this process goes awry, the neural tube does not close completely, and severe birth defects can result. Beyond that needed to prevent NTDs in early pregnancy, folic acid throughout gestation has been linked to neurocognitive development.
Good dietary sources of naturally occurring folate include dark green leafy vegetables, asparagus, citrus fruits, legumes, and beans. Foods fortified with synthetic folic acid include cereals and grain products. The recommended folate intake during pregnancy is 600 micrograms per day.
Consider this: Most women do not know they are pregnant by the time the neural tube is formed. For this reason, all women of childbearing age are recommended to take a multivitamin that includes folic acid. According to the March of Dimes, 70% of NTDs could be prevented with folic acid supplementation.
Iron: The Transporter of Oxygen to the Developing Brain
Did you know that the blood volume of a pregnant woman increases by about 50% from conception to 8½ months of pregnancy? Iron is a mineral that plays a critical role in red blood cell division and is essential for the synthesis of hemoglobin. This protein transports oxygen in the blood and to the developing fetal brain. The fetus acts as a parasite, assuring its own production of hemoglobin by drawing upon maternal iron stores, placing the mother at risk for iron-deficiency anemia, and increasing her chance of developing toxemia, labor and delivery complications, and delivering a preterm or low-birth-weight infant. Iron deficiency in the first trimester can lead to alterations in brain development, triggering long-term effects such as poor performance on childhood developmental scales.

Iron in foods naturally occurs in two primary forms: heme iron and non-heme iron. The heme form is more readily absorbed. Animal products contain both forms of iron, whereas plant-based sources provide only non-heme iron. Good dietary iron sources include red meat, poultry, beans, lentils, spinach, and fortified breakfast cereals. Vitamin C can increase iron absorption from plant sources, and it is found in foods such as citrus fruit, tomatoes, bell peppers, kiwi fruit, and strawberries. The recommended intake for iron during pregnancy is 27 milligrams per day.
Practical tip: A spinach salad is a great source of non-heme iron; top it with vitamin C–rich strawberries and a citrus salad dressing to enhance iron absorption!
Iodine: The Link Between Thyroid and Brain Development
Iodine is a mineral that plays a role in thyroid hormone synthesis. Iodine requirements increase during pregnancy to support thyroid function and, in turn, brain and nervous system development. During the first half of pregnancy, neuronal migration and myelination (aka neurodevelopment) of the fetal brain are dependent on thyroid hormones. Iodine deficiency can lead to impaired brain function and development, resulting in stunted growth, language delay, behavioral problems, and reduced motor skills.
Many countries worldwide have introduced iodized salt to correct iodine deficiencies; however, deficiency still occurs primarily in those locations that have not adopted salt fortification. Foods naturally containing iodine include fish, shellfish, dairy, seaweed, eggs, liver, and chicken. Women living in regions not known for consuming seafood and seaweed or with iodine-deficient soils/grazing pastures may also be at higher risk for iodine deficiency. The American Thyroid Association recommends a daily intake of 250 micrograms of iodine during pregnancy.
Omega-3 Fatty Acids: The Brain-Building Powerhouses
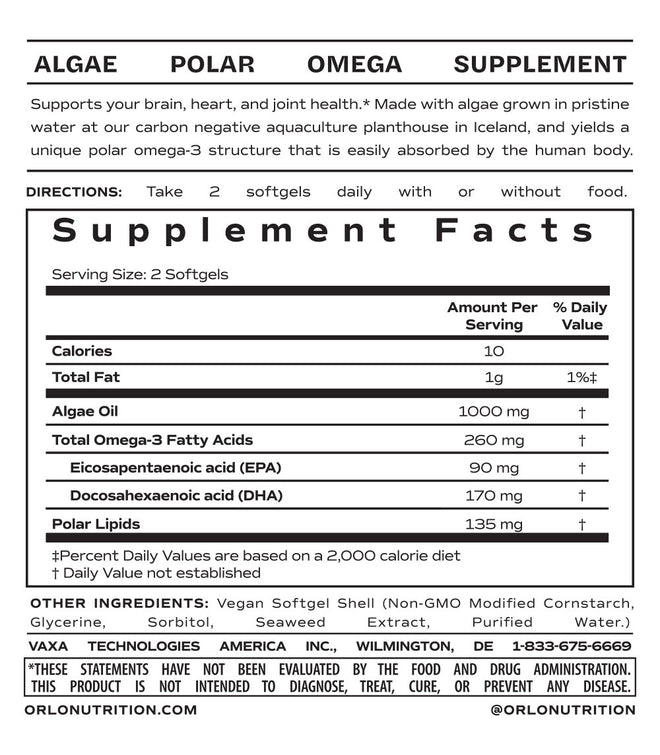
Omega-3 fatty acids support the development of the fetal brain, eyes, and central nervous system. In fact, docosahexaenoic acid (DHA) constitutes 90% of the structural fatty acids in these tissues. Omega-3s help form nerve cell membranes, support the maturation of brain synapses, and promote myelination, which is a key part of nervous system development. Throughout the third trimester of pregnancy, DHA is passed to the fetus through the placenta, an action that has been linked to the development of an infant’s brain and eventual ability to learn, judge, and concentrate. However, further research is needed to clarify the role of omega-3s in terms of optimizing cognitive function.
The primary source of dietary DHA is fish and seafood, with a small amount of alpha-linolenic acid from plant oils also being converted to DHA. Certain brands of eggs and milk are also fortified with DHA. Although there is no official recommended daily intake for DHA, several expert panels in the US recommend at least 200 milligrams per day. For those women who adhere to a plant-based diet, have an aversion to the smell of fish or burp-back from fish oil supplements, or who choose to limit fish intake during pregnancy because of a fear of exposing the fetus to heavy metals, such as mercury, adequate intake of DHA during pregnancy can be challenging.
Practical tip: Taking an algal DHA supplement, such as Active Prenatal DHA + EPA from ÖRLÖ, provides a mercury-free, vegan source of easily absorbed DHA with no burp-back or aftertaste.
Choline: The Cognitive Booster
Choline, an essential nutrient closely related to the B-vitamin family, is a key player in the development of healthy neurocognitive functions during pregnancy. These functions, including social cognition, learning, language, and memory, are linked to specific pathways in the brain. Choline is a precursor for acetylcholine, a neurotransmitter that promotes mental alertness and healthy nerve impulses. Low maternal choline intake has been associated with an increased risk of NTDs.
Choline is found mostly in animal foods such as eggs, dairy, chicken, fish, and beef. Plant-based sources include beans, nuts, seeds, and cruciferous vegetables such as cauliflower and Brussels sprouts. The recommended adequate intake for choline during pregnancy is 450 milligrams per day.
Key Takeaways:
From conception to birth, good nutrition fuels the miraculous feat of developing and growing a healthy baby. Consuming a wide variety of nutrient-rich whole foods is critical for providing the solid nutritional foundation necessary for nourishing fetal brain and nervous system development. Women who are pregnant or considering becoming pregnant should consume adequate levels of folic acid, iron, iodine, omega-3s, and choline, all essential nutrient building blocks necessary for nourishing the mind-to-be.
Additional Resources:
Podcast episode: Prenatal Nutrition: How To Nourish Your Body Early In Your Pregnancy Journey With Tia Walden
Blog: The Critical Role of Prenatal Vitamins
Blog: Essential Hormonal Health For Women
Product Referenced: Active Prenatal DHA + EPA
Note: The information presented in this article is for general educational purposes only and is not a substitute for medical advice. For a personalized plan, please consult with your health care provider or a registered dietitian.
References
Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017 Mar;27:315-389. doi:10.1089/thy.2016.0457
Caffrey A, McNulty H, Rollins M, et al. Effects of maternal folic acid supplementation during the second and third trimesters of pregnancy on neurocognitive development in the child: an 11-year follow-up from a randomized controlled trial. BMC Med. 2021;19(1):73. doi:10.1186/s12916-021-01914-9
Cortés-Albornoz MC, García-Guáqueta DP, Velez-van-Meerbeke A, et al. Maternal nutrition and neurodevelopment: a scoping review. Nutrients. 2021;13(10):3530. doi:10.3390/nu13103530
Derbyshire E, Obeid R. Choline, Neurological development and brain function: a systematic review focusing on the first 1000 days. Nutrients. 2020;12(6):1731. doi:10.3390/nu12061731
Gould JF, Treyvaud K, Yelland LN, et al. Seven-year follow-up of children born to women in a randomized trial of prenatal DHA supplementation. JAMA. 2017;317(11):1173-1175. doi:10.1001/jama.2016.21303
Iodine. Linus Pauling Institute Micronutrient Information Center, Oregon State University. Updated May 2024. Accessed September 18, 2024. https://lpi.oregonstate.edu/mic/minerals/iodine
Lehner A, Staub K, Aldakak L, et al. Impact of omega-3 fatty acid DHA and EPA supplementation in pregnant or breast-feeding women on cognitive performance of children: systematic review and meta-analysis. Nutr Rev. 2021;79(5):585-598. doi:10.1093/nutrit/nuaa060
Monk C, Georgieff MK, Osterholm EA. Research review: maternal prenatal distress and poor nutrition - mutually influencing risk factors affecting infant neurocognitive development. J Child Psychol Psychiatry. 2013;54(2):115-30. doi:10.1111/jcpp.12000
Obeid R, Derbyshire E, Schön C. Association between maternal choline, fetal brain development, and child neurocognition: systematic review and meta-analysis of human studies. Adv Nutr. 2022;13(6):2445-2457. doi:10.1093/advances/nmac082
Marci Clow is a registered dietitian nutritionist and the founder of Clowt Content, an organization which provides evidence-based content on a wide range of food and nutrition topics. The information presented here is intended only to be educational and provide readers with information; it is not an endorsement of the writer for any particular product. These statements have not been evaluated by the Food and Drug Administration. Dietary supplements are not intended to diagnose, treat, cure, or prevent any disease.