Free shipping on purchases over $69
The Low-Down on Menstrual Cramps
Written by: Marci Clow, MS, RDN
Throbbing and cramping in the lower abdomen, known as menstrual cramps or dysmenorrhea, is a normal part of the menstruation cycle. For many women, the discomfort is merely annoying, but some women experience severe pain that can interfere with everyday activities for a few days each month. This article will delve into some common causes and typical symptoms and will provide tips on how to tolerate those pesky monthly menstrual cramps.
What Causes Menstrual Cramps?
Menstrual cramps are initiated by hormone-like substances, called prostaglandins, that affect bodily functions, including the inflammatory response, pain, and uterine contractions. When the uterus contracts, its endometrial lining is shed, producing a period. Primary dysmenorrhea is the medical terminology used to describe menstrual pain that occurs in the absence of an underlying disease. There is no “normal” when it comes to menstrual cramps; they differ widely in severity, and reports suggest a variation in occurrence from 40%-90%, which tends to lessen with age and often improves after giving birth. Increased levels of prostaglandins are associated with severe menstrual cramps. Secondary dysmenorrhea, pain, heavy bleeding, and other symptoms can also occur because of an underlying pathological cause such as:
● Endometriosis: An inflammatory condition that occurs when endometrial tissue grows outside the uterus, most commonly on fallopian tubes, the tissue lining the pelvis, or the ovaries.
● Adenomyosis: Slightly different from endometriosis, adenomyosis is characterized by tissue growing into and thickening the walls of the uterus.
● Uterine Fibroids: Non-cancerous growths that grow in or on the wall of the uterus.
● Pelvic Inflammatory Disease: A bacterial infection of the female reproductive organs.
● Cervical Stenosis: This condition occurs when the opening of the cervix narrows, impeding menstrual flow and causing uterine pressure.
● Polycystic Ovary Syndrome (PCOS): A hormonal disorder affecting women of reproductive age and characterized by irregular periods.
What Are the Symptoms of Menstrual Cramps?
The tell-tale sign that your period is coming soon is a dull throbbing ache in the lower abdomen. This cramping tends to start a day or two before your period and subside within a few days. Some women also experience pain that radiates to the lower back and thighs. Menstrual cramps can differ in severity, being a mild annoyance for most women to so debilitating they interfere with daily activity.
Premenstrual syndrome (PMS) is a group of symptoms related to the menstrual cycle, which some women experience monthly, occasionally, and some don’t experience at all. Typically, PMS symptoms occur a few days to a week before the period starts and then subside. Symptoms of PMS can be physical, emotional, or both and can change from month to month.
Physical symptoms of PMS might include:
● Breast tenderness
● Headaches
● Nausea and/or vomiting
● Fatigue
● Gastrointestinal upset/bloating
● Changes in sleep patterns; increased fatigue or insomnia
● Acne flare-ups
● Food cravings or changes in appetite
Emotional symptoms of PMS might include:
● Brain fog or trouble concentrating
● Feeling sad, anxious, irritable
● Diminished interest in usual activities
● Mood swings
What Are the Risk Factors for Menstrual Cramps?
Whether or not, or to what extreme, a woman will experience menstrual cramps or PMS is hard to predict; it is different for everyone. Typically, younger women and those who start their period before the age of 12 are at a higher risk for cramps, the intensity of which tends to weaken with age. Those with close relatives who suffer from severe cramps and those who are overweight are more likely to have an increased risk. Additionally, lifestyle risk factors that can impact menstrual cramping include poor diet, lack of physical activity, smoking, and an increase in mental stress.
Is It Possible to Avoid Menstrual Cramps?
Unfortunately, there is no way to completely derail menstrual cramps. However, there are healthy lifestyle considerations that can promote overall health and may impact menstrual cramp intensity.
● Consume a nutrient-rich, varied diet with a wide variety of fruits, vegetables, whole grains, and lean proteins while reducing intake of ultra-processed foods, sugar, alcohol, sodium, and caffeine.
● Keep moving! Regular physical activity has been found to reduce mood swings, pain/cramps, and fatigue associated with menstrual cycle. Shoot for 30 minutes of moderate physical activity five days per week.
● Get your Z-z-z-z’s and allow your body to recharge. Less than seven hours of sleep per night has been deemed inadequate for most adults and has been linked to the obvious problem of fatigue, along with adverse health outcomes ranging from stress and anxiety to changes in metabolism.
What Are the Treatment Options for Menstrual Cramps?
Even though there is no magic wand to prevent menstrual cramps, the good news is there are many readily available remedies. Always check with your healthcare practitioner to find out what might fit best for your particular needs before trying any new treatment options.
● Over-the-counter (OTC) medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used as pain relievers and may help with menstrual cramping. Always follow the packaging instructions and, again, check with your healthcare provider or pharmacist if you have questions.
● Prescription medicines: Some healthcare providers may prescribe hormonal treatments, such as contraceptive pills, to help regulate menstrual cycles and ease associated symptoms.
● Alternative therapy: What works for one person may not work for another, but there are many “natural remedies” that many women swear by to alleviate cramping during their time of the month. The following is a brief description of some of the most regularly reported treatment alternatives to OTC or prescription meds:
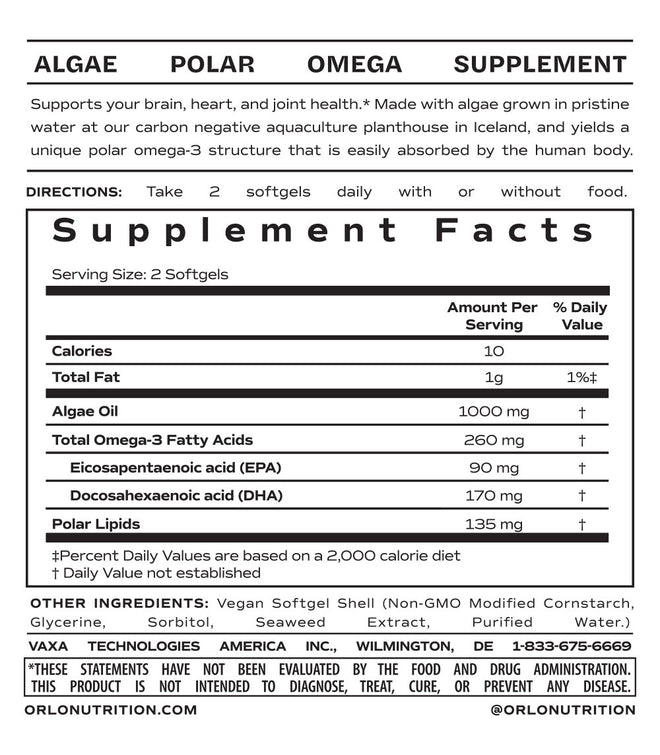
o Omega-3 Fatty Acids: The role of omega-3 long-chain polyunsaturated fatty acids in supporting a healthy inflammatory response has given way to their use as a common supplement for alleviating menstrual cramps. A 2024 systematic review and meta-analysis, aiming to explore the effect of omega 3s on prostaglandin levels and pain severity in women who regularly experience dysmenorrhea, found that daily supplementation of 300-1800 mg daily over 2-3 months was well tolerated, reduced intensity of menstrual pain, and decreased frequency of NSAID use.
o Other Dietary Supplements: From herbs used in Traditional Chinese Medicine, such as Chaste Tree (Vitex) and fennel, to the more mainstream vitamin D and the mineral magnesium, there is a wide range of dietary supplements that are used as adjunct treatments for lessening menstrual cramps. However, given the inconsistencies and, in some cases, scarcity of research, more studies are needed to verify the safety, effectiveness, and dose of each individual supplemental ingredient or combination thereof. Be sure to, yet again, ask your healthcare practitioner before using any dietary supplement.
o Heat: Consider using a heating pad or hot water bottle on the lower back or abdomen, perhaps even a soothing hot bath?
o Exercise: We mentioned regular exercise as a possible means to decrease the intensity of menstrual cramps; even light exercise, such as walking, is a great option.
o Meditation and yoga: These types of relaxation practices can help your whole body chill out, can reduce stress and anxiety, help you sleep better, and potentially improve the intensity of menstrual cycle discomfort.
o Massage and acupuncture/acupressure: Many women utilize regular massage or acupuncture treatments as a means to take the edge off and in some cases these treatments can mitigate menstrual cramp pain.
When Should I See a Healthcare Provider?
Any woman suffering from menstrual cramps should listen to their body, and if something feels out of the ordinary, never hesitate to contact your healthcare provider to see if you need to go in for an assessment. Some general guidelines
for when to see a provider include if:
● Monthly cramps are severe enough to impact your daily activities
● Your “typical” symptoms worsen
● You have heavy or unusual bleeding
● You experience severe pain with nausea, vomiting, fever, or chills
● Your period becomes irregular
Key Takeaways
Menstrual cramps are experienced by most women of reproductive age and are a normal part of the menstrual cycle. Although not completely avoidable, a wide variety of lifestyle modifications and treatment options can help make that time of the month more tolerable so you don’t have to suffer silently. If you or a loved one are experiencing menstrual cramping that prevents you from normal activity, such as school or work, make sure to contact your healthcare provider to address potential other underlying conditions and to discuss treatment options.
References
Duman NB, Yıldırım F, Vural G. Risk factors for primary dysmenorrhea and the effect of complementary and alternative treatment methods: sample from Corum, Turkey. Int J Health Sci (Qassim). 2022;16(3):35-43.
Grandi G, Ferrari S, Xholli A, et al. Prevalence of menstrual pain in young women: what is dysmenorrhea? J Pain Res. 2012;5:169-174. doi:10.2147/JPR.S30602.
Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21(6):762-778. doi:10.1093/humupd/dmv039
Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2014;36:104-13.
doi:10.1093/epirev/mxt009
Sanchez BN, Kraemer WJ, Maresh CM. Premenstrual Syndrome and exercise: a narrative review. Women. 2023;3(2):348-364. doi: 10.3390/ women3020026
Snipe RMJ, Brelis B, Kappas C, et al. Omega-3 long chain polyunsaturated fatty acids as a potential treatment for reducing dysmenorrhoea pain: systematic literature review and meta-analysis. Nutr Diet. 2024;81(1):94-106. doi:10.1111/1747-0080.12835
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-844. doi:10.5665/sleep.4716
Yu WY, Ma LX, Zhang Z, et al. Acupuncture for primary dysmenorrhea: a potential mechanism from an anti-inflammatory perspective. Evid Based Complement Alternat Med. 2021;2021:1907009.
doi:10.1155/2021/1907009
Marci Clow is a registered dietitian nutritionist and the founder of Clowt Content, an organization which provides evidence-based content on a wide range of food and nutrition topics. The information presented here is intended only to be educational and provide readers with information; it is not an endorsement of the writer for any particular product. These statements have not been evaluated by the Food and Drug Administration. Dietary supplements are not intended to diagnose, treat, cure, or prevent any disease.