25% Off - use code: HOLIDAYS
Master Your Stress: Recover From Stress, Protect Your Health, And Take Back Your Life With Dr. Doni Wilson
Watch the episode here
Stress is like a termite that slowly eats away your tree of life. How can you master your stress? In this episode, Dr. Doni Wilson, a Naturopathic Doctor, describes the different types of stress and strategies to overcome health challenges caused by stress. Dr. Wilson explains why understanding how your stress system works is essential to recover from stress exposure. When you can identify the problem, you can identify the solution. She also dives into the nutrition humans need for different stress types. Tune in to this episode to Master Your Stress, Reset Your Health with Dr. Doni Wilson.
Key takeaways from this episode:
- What are the different stress types
- Highlights from Dr. Doni Wilson’s book, Master Your Stress, Reset Your Health
- How to overcome stress
- Tools that can help with the stress response
- Nutrition our body needs to deal with stress
Guest Social Links:
Website: https://doctordoni.com
Instagram: https://www.instagram.com/drdoniwilson/
---
Master Your Stress: Recover From Stress, Protect Your Health, And Take Back Your Life With Dr. Doni Wilson
We're going to wrap up our discussion around stress for Stress Awareness Month, a coverage that is what I should probably call our pièce de résistance, as a French would say. I call it the icing on our proverbial cake. I'm thrilled to be joined by Dr. Doni Wilson. She is a Naturopathic Doctor, Certified Professional Midwife, Certified Nutrition Specialist, and bestselling author of Master Your Stress, Reset Your Health. If you haven't picked this book up, I encourage you to do so. It is an incredible read with very practical tips.
For more than 22 years, she has helped thousands of patients overcome health challenges and achieve wellness by using specific strategies that address the whole body and ultimately resolve the underlying causes of distress. Dr. Doni herself suffered from migraines for over twenty years. In the process of solving them, she developed her stress recovery protocol. Dr. Doni brings awareness to the impact of stress on our health and how it is possible to recover from burnout and set ourselves up so that we don't experience it again.
She has been featured in the media and at public and professional events for a long time. You can find her blog, her podcast called How Humans Heal, and her Self CARE Program on DoctorDoni.com. Before I bring her on, I want to remind all of you that this show is offered for educational and entertainment purposes only. We are here to inform you, but if you have specific health concerns, you will want to connect with a qualified medical professional, and perhaps that's even Dr. Doni herself. Dr. Doni Wilson, welcome to the show.
Thank you so much. I'm glad to be here.
I'm so thrilled that Dr. Shawn Tassone put us in touch. I've enjoyed collaborating with him thus far, getting a chance to listen to your podcast and some of your guest appearances, and getting about halfway through your book. I am quite primed and excited about this conversation. I would like to start first by learning a little bit more about the origin story that you have of what brought you into naturopathic medicine and how you've used your personal experience with battling migraines to inform your work.
Thank you so much for asking. Even my inspiration in this direction of natural healing started from my childhood. My father was a pharmacist. I grew up in the pharmacy and was always around the pharmaceutical industry. At the same time, my mom is a special education teacher. I remember my mom saying to me as a kid as if she was explaining to me what was going on in the day. For example, she would say, "That person is stressed." Maybe she would say to me I seem stressed.
I had this concept of feeling stressed in my awareness even from a young age. When I went to do a pre-Med degree, I was very interested in nutrition and ended up getting a Nutrition degree as well. I had this thought as a college student, "What if there was a type of medicine that used food as medicine?" That's a novel thought in a pre-Med degree. That's when I learned about naturopathic medical school. There are now 5 or 6 in the US and a couple in Canada naturopathic medical schools that have in-the-institution training, followed by board exams and residency.
I went to Bastyr University and graduated in the year 2000. Even during my training as a naturopathic doctor and a midwife, I was experiencing migraines. I was trying everything. As a naturopathic medical student, you try every detox, supplement, herb, and modality. Some of them made me a little bit better, and some of them made me feel worse, but none of it completely took away the migraines. I started my practice. I moved from the West Coast of the United States to New York.
I moved to Manhattan right after 9/11. I was moving into a hugely stressful environment while coming out of medical school and experiencing migraines. I was a new mom, also. First of all, I was very curious about how stress affects humans. I was curious about how we could heal using all of my training and how to help my patients. At the same time, I was experiencing these migraines and trying to solve them myself, but I wasn't telling anyone. I felt like an imposter. As a naturopathic doctor, I shouldn't be experiencing migraines. I was solving it but at my time in the background.
It inspired me to learn so many things over the years in my practice to dive into understanding cortisol, neurotransmitters, food sensitivities, leaky gut, and gluten sensitivity, as well as MTHFR and gene variations. The migraines inspired me to learn so much that I was then able to apply them to my patients. For the past several years, I don't get those migraines anymore, but I'm grateful for them because they drove me to learn everything that I've learned to help other patients.
From personal experience, I've had five migraines in my time. Often people call a headache a migraine, and it's not exactly the same thing. I was getting to the point where I needed to be in a cold and dark room with a towel on my head. I would probably end up so nauseous. I would end up vomiting as a result of the migraine itself. That's never a comfortable position to be in but I personally always saw it as a marker that I needed to address something in my life.
I didn't seek pills to solve it. I sought a resolution to the stress. The thing that I noticed every time that one erupted was that I was taking on too much. The first one occurred when I was volunteering at a horse ranch on Sundays in addition to taking a six-week intensive language course. I was in 30 hours of class a week, studying for exams, and working full-time. It was too much. That first migraine came on when I was driving away from having volunteered for the day in the hot sun at this horse ranch.
Looking back, you're like, "I got a migraine."
You learned a little bit. For me, it was so obvious. I overloaded my plate. There was no space for me to heal while I slept even, which is something that you dive into in your book as well. I want to point to this because it spoke to me when I read your book. You are saying, "I wrote a book about sleeplessness or insomnia, but I didn't do that until I was able to get seven and a half hours of sleep a night." You had proven that you could conquer it in yourself first and could, therefore, confidently stand behind the work you had put into the world. That speaks to me. It means that you're coming from a very genuine place. You're going first to solve it for yourself before you feel comfortable enough to share that with the greater world.
I do feel that way. I'm so inspired to write and help people, but I feel very strongly that I'm going to try it on myself first, and I'm going to going to be walking the talk before I encourage anyone else to walk that same path. I do everything I write about. It's because I've tried it on myself and found that it was helpful, and then I've tried it with my patients and had their feedback that it was helpful. That's missing in a lot of healthcare. Even in the natural medicine world, sometimes that's missing. Sometimes we hear things are, "You should do this," but is the person saying it doing it themselves?
Here's a point-blank question. Is stress the root cause of migraines?
Yes. The thing is that I look at it as no matter what health issue we're looking at, whether migraines, autoimmunity, or anything, we know that it's a combination of genetics and stress exposure. It always comes down to that because stress is not just psycho-emotional stress. I'm referring to stress as also infections as stress, toxins as stress, and lack of sleep as stress. Anything that's happening in our environment that's not healthy for our bodies is stress.
Anything that's happening in our environment that's not healthy for our bodies is stress.
Genetics is the other piece. While researching genetics, I found that genetics plays very much less of a role than we would think. We used to think that genetics was 100% of the determiner of our health, and now we know that genetics is less than 10% of the determinant of the health outcome that we're experiencing. Genetics does play a role, but what's also so interesting is what turns on our genetic predispositions is stress. It's right back to stress again. If you say to me, "What's the main cause of any health issue?" I'm going to say it's mostly stress. There's only a small percentage of it that's genetics.
Sometimes eating food that is not right for your body creates stress as well. It's an inflammatory response in your body, which creates more stress and cortisol. What do you do in those situations? You have to address the stress. Let's talk about this for a moment as we open the discussion. What is the role of the adrenal glands themselves as it relates to stress and then how cortisol comes into play? People can have hyper-low cortisol or high cortisol in terms of stress, which is confusing to me too.
That's the thing. When people hear that so much of our health is determined by our different stress exposures, sometimes then, we almost throw in the towel and give up. I'm hoping that your audiences are getting the message. This isn't about giving up, and it isn't about trying to have zero stress, either. There are certain stresses that are stress that we want. We're not saying that we're trying to get to zero stress, and we're not saying you have no chance here up against stress.
We're saying there's so much we can do to help you recover from stress exposure that it's worth putting your attention there. Understanding how stress affects us is the beginning of that. No matter what I'm trying to solve in my daily life, if I first understand the problem, then I'm much more likely to be able to solve the problem. Understand how our stress system works. We have a built-in stress system as humans. It's built-in. We don't have to get one at the store, but part of our stress system is what we think of as a fight or flight system that's known as this sympathetic nervous system.
Let's say the alarm goes off, and you feel your heart racing. That's the sympathetic nervous system or a fight or flight system making adrenaline to get you out of danger. We need to have a healthy ability to protect ourselves and get out of danger. The second step of that stress response is when the brain sends a signal to the adrenal glands, which you mentioned. The adrenal glands make more adrenaline, and they also make our main stress hormone called cortisol.
We have a stress signal going throughout every part of our body. Every cell gets the memo, "There's a stress happening." They get the memo from the adrenaline and the cortisol. This is a good response if there's acute stress happening and you need to get out of danger. The problem is that it should turn off but in our modern lives, we're having so many stresses constantly that the off signal stops working. We end up in a constant stress response. It's in that constant stress response that we have a more individualized outcome. The cortisol and adrenaline levels at that point look different for you than for me.
I can't recall where I heard this first, but somebody else speaking on stress compared it to a gazelle running from a lion. The gazelle runs away. That immediate flight response kicks in. They're bounding away with a burst of energy. When they get out of range, they don't turn around, stare at the lion, and continue to be stressed. They shimmy off the stress response in their body and then return to grazing. We have lost that connection to be able to easily do that with a snap of a finger. What types of tools can support that or that you find most successful for your patients or in your life?
How do we emphasize stress recovery? How do we help reset that stress response? Ultimately, what's considered optimal health associated with longevity for humans is when we can turn on and off our stress response. It shows up in the heart rate variability. You've spoken about that. Some people are aware of the ability. With a device, you can measure slight variations in your heart rate. Those variations in heart rate are associated with the ability to respond and recover from stress.

To your question, how do we help our bodies? How do we build that muscle of the recovery response? It comes back to some things that might seem way too simple, including taking a deep breath. Sometimes we hear that if someone is stressed, someone will say, "Take a breath." It almost annoys the person more. Anyone listening could try it. When you take a deep breath, you are signaling to the opposite part of your nervous system from the fight or flight. You're signaling to the parasympathetic nervous system and the vagus nerve, which communicates the anti-stress signal throughout your whole body simply by taking a couple of deep breaths.
Sometimes it's a matter of becoming more aware of when the stress response is happening and reminding ourselves, "Maybe I need to take a couple of minutes and take a couple of deep breaths." It's what you said about animals. They shake it off, even the dog. My dog barks. When whatever she's barking about is done, then she shakes. We need to move, shake, take a walk, or get out in nature. This is where we even can go into things like mindfulness, meditation, breathwork, and music. There are so many tools that we know help to reset and teach our bodies, "This is how you reset from stress."
Another thing that you mentioned in your work is the fact that even getting more restful sleep can help us better recover more quickly. I know that you've done a lot of work in the realm of insomnia as well as helping people recover from that. I wonder if we could talk for a moment about the role that sleep plays in this whole system working better so that we can recover from these moments.
I finally realized it for myself because I was also brought up to get lots done. We have a long to-do list. There's so much to do. We need more hours in the day. We start stealing from our sleep hours to get more of our to-do list done. With that, we're assuming that we're doing nothing while we're sleeping. We're like, "If I'm sleeping, I'm inactive. Nothing on my to-do list is getting done." What I started realizing the more research I read about sleep is that there's a whole lot of stuff getting done while we sleep.
When I remind myself of that, then it shifts the game completely. I'm like, "I need to get myself in bed and get to sleep because my body has a whole long to-do list of things to do while I'm sleeping." There are all kinds of glymphatic brain cleanout and memory generation, let alone all kinds of autophagy, cellular cleanout, and repair that happens while we're sleeping. It becomes more of a priority. Once we see it as a priority, then we start to shift our daily routine to appropriately give it the time it needs.
Many people are night owls. They like to stay up late, but you also make the point in your book of getting enough sleep between the hours of 11:00 and 3:00 or ensuring that you're able to go with some of the natural rhythms of our environment, the sunrise and sunset, and the circadian rhythm. This can be a problem for people living in Northern latitudes, especially in the summer. I have a niece who lives in Alaska, for example, and friends who live in Scandinavia where it's light 24 hours a day. It can be very confusing to your circadian rhythm. What do you recommend in those cases where people might be living in the extremes?
Some of us who are in winter darkness a lot of the time end up putting lights on. We have this artificial light at all different hours. We're working the night shift or traveling and changing time zones. There are so many ways that we, as humans, can scramble our circadian rhythm. It's about realizing we're living in human bodies that are so responsive to nature and the fact that we live on Earth that does have a natural dark and lightness cycle. If we lose touch with that, it's going to throw off a lot of different systems in our bodies.
We're living in human bodies that are so responsive to nature. If we lose touch with that, it will throw off a lot of different systems in our bodies.
What I recommend is no matter where you are in light and darkness, look at your daily schedule and make a plan. Set it on your phone or whatever reminder you need to have. Make a bedtime routine alarm. That's what I do. I was like, "At 9:00 PM, I need to be turning down the lights or maybe even earlier at 8:00 PM if I can." If it's light out, turn out the lights. Maybe you need to get blackout curtains if it's still light outside. Create as much darkness as you can in your space and at least in your bedroom so that you can give your brain the perception of darkness.
Luckily, there are now a lot of ways that we can do that. It's the same thing with light, though. When we wake up in the morning, we need to give our brains a perception of light exposure, whether we go outside or put on some light. There are a lot of lights that are made to help people with Seasonal Affective Disorder so that they get light exposure in the daytime. There are ways that we can help to say, "Here's the light when my brain needs to perceive light and darkness. Let's create that in our daily routine."
I'm glad that you touched on this because many people, especially in the Northern latitudes, will turn to certain supplements like Vitamin D to ensure that they're getting enough of that sunshine vitamin. What other nutrition perspectives or things that are of good nutritional support can ultimately help us ensure we get better sleep and also better sleep hygiene and reduce our stress? Are there any tips you have in this arena?
I always think it's cool to think that even if you're laying in bed and your eyes are closed, but the room is dark, our brains are able to pick up on that darkness and stimulate melatonin production. That's one of the key things why you want darkness. I even try to put out and cover any little lights in the bedroom. You don't want any light. You want your brain to perceive darkness when you're sleeping so the melatonin is released. Melatonin is made from serotonin, and serotonin is mostly made in our gut or our digestion. Serotonin is made from the amino acid 5-HTP, which comes from tryptophan.
I bring it all the way back to protein in your diet. I find that so many people are not getting enough protein in their diet, and they're not realizing it. If we're not getting enough protein, we're not getting enough amino acids. Those amino acids are not only important for muscle building. They're also important for liver detoxification. They're essential for making neurotransmitters like serotonin, which converts to melatonin. You start to go, "My sleep is impacted by what I'm eating during the day, and not only that, but how well I'm digesting that food and how well I'm absorbing those nutrients."
When you speak to tryptophan, most people think of turkey, but you mentioned protein in general. Can you expect a certain level of tryptophan to be in most animal-based proteins? What about the plant-based ones themselves?
Animal-based proteins tend to have a good array of essential amino acids. We usually think of turkey as particularly high in tryptophan, but there is tryptophan in other animal proteins as well. This is one of the things. There's research on the benefits of having a plant-based diet, but there are also challenges like anything. This is why I always say, "There's such a thing as too much of a good thing." A plant-based diet is great because it's bringing us back to awareness of getting whole fruits and vegetables from nature versus relying on processed foods and fast food.
A plant-based diet is great because it's bringing us back to awareness of getting whole fruits and vegetables from nature versus relying on processed foods and fast food.
I look at a plant-based diet in contrast to going to fast food restaurants and living on hamburgers and cheeseburgers. That's the contrast but then what I'm doing is I'm looking at a 100% plant-based diet, which I do for certain periods of time every year, I follow a plant-based diet. It's that I also want to be aware that on a plant-based diet, it can be harder to get enough amino acids in the protein. It can also be harder to get enough iron, B12, and folate. We need to be aware that if we're going to choose a diet that's a little bit more extreme, how do we still make sure we're getting adequate nutrition?
That's such a critical point. To bring it right back to tryptophan, there isn't a plant-based source of tryptophan.
I can't say, "Eat this." Most of my patients are fully plant-based. I measure neurotransmitter levels. I see when my patients have low serotonin levels. I recommend a supplement of 5-HTP because then you can get the precursor nutrient 5-HTP, and your body can then make more serotonin directly from it. To me, that's a recovery tactic. I'm seeing there's low serotonin in phase one of my stress recovery protocol. Let's address that deficiency. This is anemia of neurotransmitters.
Let's address it and use 5-HTP to get the levels back to optimal, but at the same time, we want to help your body and your diet so that you are getting more amino acids in your diet. You're able to digest that protein and absorb those nutrients without triggering inflammation from a leaky gut, and the gut bacteria are balanced so that your gut is a healthy producer of neurotransmitters for you. You're not going to become deficient again.
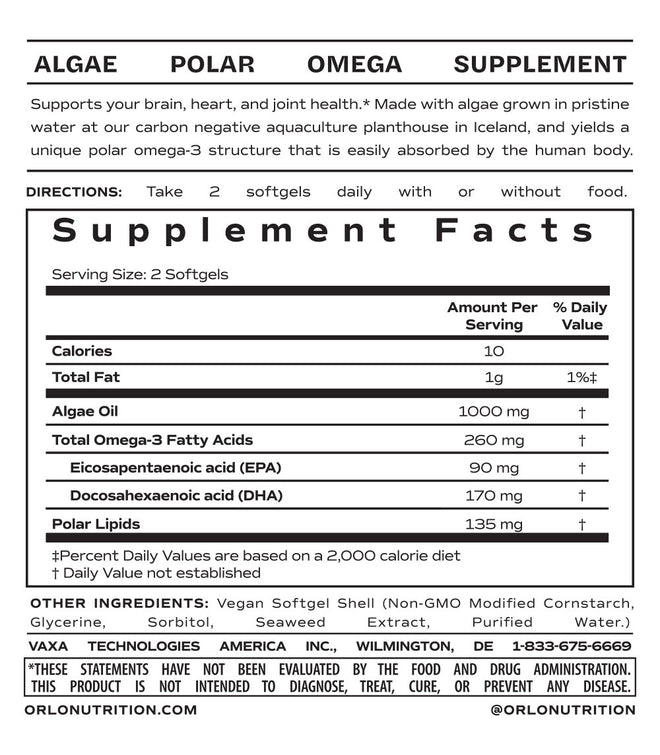
To your point, Vitamin B12 and even Vitamin D3 are common deficiencies in people, even if they aren't vegetarian or vegan. Check your levels and then find the right supplement if you're not going to do something like eat organ meats, for example, to get your iron and your Vitamin B12. Thankfully, at Orlo, our spirulina itself produces Vitamin B12 in the methylcobalamin form. It's the methylated form.
I want to clear something else up because this has come up for me personally in a couple of different conversations, one of which I was speaking to Dr. Joel Fuhrman, who is MD and runs a practice in San Diego where he helps people recover from all sorts of health conditions through diet and lifestyle changes. He mentioned that we shouldn't be taking multivitamins with folic acid in them.
I want to touch back to this because I don't think people understand the B vitamins as well as perhaps they should, and folate versus folic acid. Women are still told all the time, "If you're prenatal health pregnant or nursing, you need to be taking folic acid or a supplement that has folic acid in it." It feels like we're behind the eight-ball. Help us understand this issue.
I agree with Dr. Fuhrman. I talk about this in the Master Your Stress book because I feel so strongly about it too. If a supplement company is going to make a multi or a B complex or put B vitamins in, that's a measure of quality. I'm immediately looking. Do they have methyl folate and methylcobalamin or methyl B12? I know that the company is paying attention to providing active nutrients that the majority of people are going to be able to use versus the companies that are using low-quality and less expensive nutrients that some of their consumers are not even going to benefit from. That's a quick check for any of you, "Is it methyl folate and methyl B12 on my multi and B complex?"
The reason is that these are the active forms of these nutrients. Even if we start with the fact that our body uses B vitamins in so many ways, sometimes you've heard about that. When we're under stress, people will say, "I'm under stress. I probably need more B vitamins." That's correct because we burn through our B vitamins so much faster when we're under stress. That's because the B vitamins are used to make adrenaline, break down adrenaline, make serotonin, break down serotonin, protect our cells and DNA, make new healthy cells, and detoxify. When we're exposed to toxins, we need more B vitamins too.

These B vitamins are doing so much good stuff in our bodies. It's no wonder that we run out when we're pushing ourselves to the max, yet we are left with, "How do I know which ones? How much do I need as an individual?" Some of it is related to genetics to some degree. You can find out. With patients, I do their genetic analysis to see their genetics related to B vitamin metabolism. For example, the gene MTHFR is related to the ability to turn folic acid into folate. At least 40% of us have a decreased ability to do that. If 40% of us are less able to use folic acid, why would we even put it in anything? Let's use the folate form that all of us can benefit from.
That's just one of the genes. There's MTRR. There are all the other genes related to B vitamin metabolism. When I dig in and look at that, what I come away with is I'm going to want to recommend for everyone to make sure if you're taking B vitamins, take the active form or the methyl form. If you are not feeling well and if you're getting migraines, you're getting anxious, or you're getting fatigue or sleep issues, then we can dive deeper. We can analyze your genes. We can test much more closely. We can look at homocysteine levels and methylmalonic acid levels and understand what it is that's blocking your ability to benefit from the B vitamins.
Are you also assessing what genome type they are, whether it be an APOE3 or APOE4?
APOE ones are associated with dementia risk. Sometimes some patients do want to know, "What is my APOE status?" What we now know is dementia is associated with a whole long list of genes, and APOE is only one of them. To me, whichever APOE status you have, some of these same strategies are going to help the same dropping inflammation, recovery from stress, and detox from toxins. This is the way we prevent dementia.
I wanted to bring that up because I've taken both the Ancestry test and the 23andMe because I wanted to find out how much Neanderthal I had. It also came with more than I anticipated insofar as expressing to me what genome type I happened to be. I did find out that I have one representation of APOE4, which wasn't a complete surprise because my grandmother also suffered from dementia.
I also learned that I had one gene for celiac. I've taken other tests to test my sensitivity to wheat and gluten in particular. It was an Everlywell test they make available for a couple of hundred dollars because I was trying to assess what I might be reacting to. I learned that even though I have that one representation of celiac, I have zero sensitivity to gluten, but I have sensitivity to other proteins in grains.
Given that, I tend to limit my consumption of grains. I'm going to eliminate rice from this. I don't seem to have any issues with rice, but when I eliminate all the other grains, I feel more connected to my gut. I can't even describe it in another way. I noticed that I also feel a little slimmer there, even if my weight remains the same. There's less inflammation happening in my gut.
These are the personal experiences I'm bringing out because I want people to understand too that if you're listening to your body, and you couple it with a couple of tests to figure out where you might have some red flags that you want to address, that can help manage your health journey. Something else I discovered through reading research on Omega-3s and connecting with Dr. Melanie Plourde from Université de Sherbrooke in Canada is that APOE4 allele individuals have a harder time assimilating Omega-3s.
If we learn that there's a connection between Omega-3s and the brain and that you might need more of these particular things to help treat a potential for a later onset of a health issue, then you can both manage your health, give yourself inputs that are better for you. Also, to be focused on getting the most bioactive form of something. Something she shared was that there's an indication, at least in early animal research, that if you're taking a polar lipid like those that we produce at Orlo or a monoglyceride, people with APOE4 genome type are having an easier time integrating those omega-3s into the brain and eyes.
The more we learn that we need to be going to the most bioavailable form, which typically comes from food or the earliest point of food, like your point of going to the animal proteins to get the tryptophan, and then go ahead and create a system that's working appropriately. If we're going to algae and getting the polar lipid that exists that the fish eats, then we're navigating the whole thing. We can even do some of this through vegan means with the algae. It's a long journey.
I love it. Omega fats are so essential. Often we miss it. A lot of times, I find people say to me they might even know that taking Omegas is good for them, but they're like, "What should I take? I'm afraid to get toxins or that it's not going to be a beneficial form." To be able to trust, "Here's a good source that's going to help and not cause a problem," is going to be huge for people.
That's where I've spent the bulk of my career studying Omega-3s because so much of this conversation has already touched on them, things like the production of energy and times of stress. You need your B vitamins, but your omegas also come into play to create that ATP pr that cellular level of energy, which is much different than relying on your coffee for an added spike.
While I do sometimes feel that doctors like yourself rob me of my love of coffee because I probably drink far too much of it, it makes sense that we shouldn't be driving to stimulants to help us push through these times of stress. We should be considering how the whole body system is working and ultimately consuming these things in balance and eating a more varied diet.
Maybe you have your cup of coffee, but you shift to tea and drink more water. I'm hoping that you can ultimately share with our audience your perspective from this greater capacity of how much we should be eating, what types of liquids we should be drinking, and when so that we can set ourselves up for the most success, not only in managing our waistlines but our stress levels and our sleep.
It is how to find that Goldilocks or that sweet spot for each individual because, as humans, we're willing to do more for longer. We're willing to push, but that's the problem because we're pushing so much that we're pushing past the hormetic zone. Hormesis is when we're giving our body a bit of a challenge or a change, but we only want to do so much change that's going to be beneficial and create a beneficial effect for us. If we push too much, now we're putting ourselves into this high-inflammation and high-exudative stress and being hard on our mitochondria again.
How do we find that? How do we identify when we're in our hormetic zone for ourselves? It does take that body awareness we have been talking about. How do we listen to our body signals more? How do we understand the symptoms that we're experiencing? How do we understand ourselves as individuals? When it comes to what I refer to as CARE, Clean eating, Adequate sleep, Recovery activities, which is even meditation, and E is for Exercise. Exercise is a perfect example of this.
We know that exercise is beneficial, but we also know that if we overdo it and if we go too intense for too long, we're increasing cortisol levels. We're increasing the risk of injury. We're working against ourselves. Say to people, "Take a breath again and realize that maybe less is more for your body." Start to realize what that is for you in terms of even quantities of food, "Here's exactly the quantity of food that I can consume at this moment in time. I know that my body is going to be able to digest it and absorb it."
"My insulin is going to be able to handle the carbs. My mitochondria are going to be able to use that energy. It's going to go smoothly. If I eat too much, I'm ending up overwhelming my digestion, overfeeding bacteria, and stimulating leaky gut and inflammation." It's the whole snowball effect. It takes practice. I end up deciding that this is what being human is. It's practicing and learning this zone where our bodies are functioning optimally. That includes cortisol and adrenaline levels. To me, that's the first thing on the list of everything. That gets missed.
We walk around doing a lot of good stuff. We're eating healthy, exercising, and meditating, but if we don't have an optimal cortisol level, it's for nothing. It's for naught because there's still an imbalanced stress signal happening in the background. We need to figure out what is your cortisol level. Is your cortisol too high at certain times of the day? Is it too low at certain times of the day? Whichever it is, we need to work on getting it back to this optimal zone because when cortisol is at optimal, everything else is easier. Everything else works better. Everything else is smoother. It's this positive ripple effect. To me, the big piece is getting cortisol to optimal.
When you're looking at optimizing something, you need to measure it. One of the things we have talked about already a couple of times is the sorts of tests that you might perform in genetic tests and also a cortisol test. This is something we touched on when we spoke with Dr. Tassone in our last episode with him. He shared that he likes to do saliva tests because you can perform them many times throughout the day. You need to check specific waypoints. What is your perspective when it comes to how best to test for stress and when to test for cortisol specifically? What does this cost? How do people ask for it? How do they access this test?
You can test cortisol and blood, but then you only get it at the time your blood was drawn. Cortisol is a hormone that should be higher in the morning and gradually decrease through the day so that it's lowest at night. To get a sense of what's happening with your cortisol, we need to measure it at least four different times a day in the morning, midday, evening, and bedtime. That can be done with saliva. That's what I usually use. A person can spit in a tube, and you can do that from home.
It can also be measured in urine. We can see your cortisol because then it might be fine in the morning but it's too high in the evening, or it's low in the morning and fine in the evening. We need to see your cortisol curve. That is not a standard test. If you go to the regular doctor's office for your annual exam, they're not going to usually do that because this is not on the radar in the standard medical approach. It's not generally covered by insurance even.
Every single person should know their cortisol levels. This is essential for health, but we have to realize that our medical system and our health insurance systems are not there for preventive medicine. They're there once a health issue develops in helping you solve it in the acute state. If we want to be preventing our health, we're going to need to take care of it ourselves. That involves, "Let me get a cortisol panel done so I can see where my cortisol levels are."
If we want to prevent our health from deteriorating, we must take care of it ourselves.
You can order that usually from what would be called someone like me, a naturopathic doctor, or a functional medicine doctor, or have different practitioners that have this training, but here's the thing. A lot of times, I find that even if some practitioners are ordering cortisol levels, they might not be doing the right treatment. I also want audiences to know that when you get your cortisol levels back, make sure then that you carefully choose the correct treatment to help optimize your cortisol. I write about this in the book because this should be general knowledge.
If cortisol is high, we're going to use different herbs. There's research on these herbs. We're going to use ashwagandha, banaba leaf, magnolia root, and phosphatidylserine, which is a nutrient. Those are known to bring cortisol down when it's too high, but we use a completely different set of herbs like rhodiola, licorice, and holy basil and different nutrients like pantothenic acid to raise cortisol when it's too low. You have to know where you're starting from to know what to take and at what time of day to take it.
That's so helpful. As far as managing the extra costs that come from some of these tests when you're trying to get a baseline and then see where you are, what do you think people can expect?
You asked me that. The one that I run is about $400. It's not just cortisol. I'm also measuring adrenaline levels and neurotransmitter levels. You get a lot of information from $400. To me, that's well worth the investment because otherwise, you might be spending $400 on the wrong supplement that's not helping you any. I would rather spend $400 and know, "This is my body's pattern." This is what I saw in my research. We each have a pattern of our cortisol adrenaline. It's almost like our fingerprint.
When I'm under stress, my cortisol and adrenaline want to go into this imbalance. By knowing what my body's tendency is, then from then on, I know this is what I need when I'm under stress. It's not like you have to be constantly rechecking it, although I would love the day when we can get a cortisol level on a device that tells us from moment to moment what our cortisol levels are. That's going to be very cool one day when that exists, but for now, what I can tell you is that, in most cases, I see patterns. That's why I call them the five stress types. Those are the five most common disruptions of cortisol levels and adrenaline levels so that you can know. You invest in a $400 test, but then you have that information going forward.
Let's quickly snapshot the five stress types because I'm about halfway through your coverage of each of these. There's a quiz in your book as well to help people at least get an idea of which stress type they might be. I was having a hard time because I felt like I identified with a few of them in different ways or at different times in my life. How about that? Let's learn a little.
Sometimes when I read them, I'm like, "I sound a little like this." There's a quiz I've developed by analyzing results and working with patients. I was able to narrow in on a quiz that is also available on my website. You could do it in under two minutes to give you a sense of what your stress type is. First, there's this Stress Magnet. The Stress Magnet tends to have high cortisol and high adrenaline either all day or part of the day. A lot of times, people assume that's them.
They're like, "I probably have a high cortisol." You might, but once you go through the quiz, I can talk you through a little bit of how I do it. You go, "Am I a Stress Magnet?" The opposite of the Stress Magnet is Blah and Blue. They tend to have low cortisol and low adrenaline for part of the day or all of the day, but the symptom of fatigue or low energy could happen in either a Stress Magnet or a Blah and Blue. It's just that Blah and Blue is more likely to experience more extreme fatigue.
There's the in-between. The Sluggish and Stressed have high cortisol with low adrenaline. The Tired and Wired has high adrenaline with low cortisol. They have slightly different symptomology and experience in their body and their life. The fifth one is the Night Owl. The Night Owl tends to have high cortisol and/or adrenaline at night either in the evening or the middle of the night. They're more likely to have either sleep issues or a tendency to have energy and stay up late at night.
It could be related to stress at home. You never know too. What would you say to someone who says, "I thrive on stress and being super busy."
A lot of people say, "I'm okay. I'm stressed, but I love it. I'm an adrenaline junkie." I tend to be a person like that too. I'm constantly thinking of new projects and doing lots of new things. I love new activities. There is some amount that's fun for humans, but there's also sometimes an addiction to it because if we're doing things that stimulate a dopamine release, for example, and dopamine turns into adrenaline, now we are addicted to stress because it's stimulating a neurotransmitter release. That feels good at first, but the real science behind it is that in the long run, it's working against you to have high adrenaline and high cortisol a lot of the time.
You might be feeling fine now, but based on research and clinical experience, at some point, it's going to start causing trouble, whether it's going to trigger autoimmunity, heart disease, dementia, or cancer even. All of these things are associated with having high cortisol and adrenaline. There's a way to still enjoy your life, be inspired, and do wonderful things, but do it with awareness for your cortisol and adrenaline and make sure that you are also giving your body a chance to reset them to optimal levels so we're not in a constant state of high-stress hormones.
You've stated that so eloquently. Thank you so much for that. In your book, you talk about how going too long without eating, especially for certain stress types, can create problems and disastrous effects of eating all at once. Many of us are hearing great things about things like intermittent fasting. We might be pushing ourselves in that direction. We perhaps took a quiz online and said, "I need to be at a 16:8," or something to that effect. How do you advise people to start approaching their eating habits, specifically if they are under a lot of stress?
I'm glad you're asking this. This is a perfect example of how once you know your stress type, then you can use that in everything you're implementing, including your diet, stress recovery activities, and exercise. Everything you do needs to have this awareness of your stress type in mind. If we go into a dietary change like fasting, it's the same thing. It's a hormetic activity.
We know that if we do some amount of fasting as humans, it can stimulate autophagy, which is cellular cleanout. It can stimulate longevity and so much positive change in the body, but if we overdo it, now we end up hitting the other side of the danger zone where it's going to work against us. A lot of times, people hear about something that sounds good, "Intermittent fasting sounds great," and it is, but there is such a thing as overdoing it.
Have that awareness for yourself and ask yourself, "Am I fasting a little too long?" The ways you will know is if you test your cortisol, and your cortisol is too high, "I'm pushing it a little too far. My cortisol is going up too high," or if you're getting bloating and digestive issues because what can happen when you have a shorter eating window is now, you're still trying to get the same amount of calories but in a shorter period of time. We might be consuming larger quantities at once.
When it comes down to it, our digestion can only digest so much food at once. If we pour in a bunch, then we end up overfeeding bacteria, which causes bloating. We're not benefiting from all those nutrients. Even if it's a healthy food, you're not even benefiting from it if you can't digest and absorb those nutrients. That's what I see a lot of times for people who are saying they're excited about intermittent fasting but maybe pushing it a little too far.
They end up noticing their high cortisol. It might disrupt their sleep. They start getting anxiety, digestive issues, hormone imbalances, and menstrual cycles thrown off. These are all signs that it's a little too much for your body, and we need to back off. To me, the definition of an intermittent fast is not eating while you sleep. That's a minimum. We're not going to eat while we're asleep. At the very least, we're all getting some amount of intermittent fasting while we're sleeping. Hopefully, you're sleeping at least somewhat during the night. If not, we need to solve that first.
Let's get you sleeping at least 7 and a half to 9 hours. You have that much of a fast even if you ate right before you went to sleep and immediately when you woke up. I start to expand it little by little, "How about we don't eat within 2 to 3 hours of going to sleep? How about you wait an hour or two to eat in the morning?" You're expanding your overnight or intermittent fast enough. That much already stimulates a positive change in the body.
We don't necessarily need to go to more extremes. Sometimes I do. I was in the Amazon. When I go to the Amazon, that's an extreme detox situation for sixteen days. I'm having two meals a day. I'm already on a very anti-inflammatory, mostly plant-based diet. In that case, sometimes I was fasting 16 to 18 hours, but I was on a very different daily schedule. I wasn't doing my usual activities or exercise.
We have to keep that in mind too. If we're going to fast longer, then we need to understand that our body is going to need more rest and more support to get through it. We probably only want to do it for a short period. When we come back to our usual day-to-day activities, we need to adjust. That's the thing. More than anything, I hope you hear from this that it's about helping our bodies to be able to adjust to the situation and have a healthy ability to respond and reset. That's what's associated with health more than anything.

I love that. The points that you make in your book as well as listening to your body, "Perhaps you need to eat more frequently or break your fast with something that is protein and fat as opposed to carbohydrate," all help us to set ourselves up for success. Even if we are doing an eighteen-hour fast, which may sound like a lot, we might be eating, in that case, every couple of hours, a smaller quantity while we're in our eating window so that we can absorb the nutrients without overloading our systems.
You're making an example in the book. Eating a ton of blueberries isn't necessarily going to give you more benefits. A quarter cup, which is a relatively small amount, or even a handful can give you the benefits of all the phytonutrients in the blueberry and also stimulate the right bacteria in your gut. Throwing more on isn't going to do a lot more for you. That can be how we help ourselves.
Something else that I hear consistently from all these incredible professionals like yourself, naturopathic and functional doctors in particular, is that protein is key. While going keto may be right for some people for a period, it may not be the best solution long term because you're getting 80% of your calories from fat and only 10% from protein and carbohydrates.
In any choice you make with your diet, you want to make that choice intentionally. I would consider that more of an extreme diet choice. You might choose to try it for a period of time for certain medical purposes, whether that's diabetes or weight loss. You might try it, but I would always want to start by saying, "Do I have a foundation first? Do I have a foundation of care? Am I good in good sleep? Are my nutrient levels balanced? Is my cortisol optimized? Have I taken care of all of these essential things? Am I prepared to go plant-based or keto for two weeks?" You're working with a solid foundation.

One of the problems with keto that we should touch on briefly is that when you are consuming that much fat, you need to work to balance your fats. It's so much easier to get omega-6s than omega-3s. Leaning on saturated fats and perhaps medium-chain triglycerides more than something like cooking oil is going to be better for you and set you up for more success. Make sure that you're getting enough omega-3s, EPA, and DHA. Orlo provides a great solution for that because they're in that polar lipid form. As we prepared to wrap, I would love to hear from you if there are any particular supplements that you say are generally good for everybody to consider taking.
I would start with making sure you're getting electrolytes, which may not even have to come from a supplement. You can get that from sea salt. Make sure you're getting filtered water and electrolytes. From there, magnesium is often deficient. I'm like, "Let's make sure we have enough magnesium." Magnesium helps us metabolize adrenaline.
If you know you're one of the stress types with high adrenaline, you feel that adrenaline and you need to help your body metabolize it, or you're getting PMS symptoms, that's another sign, then let's make sure you're getting some good magnesium. There are different kinds of magnesium. I can go into so much about that, but I would be thinking more of magnesium 3 and 8 and glycinate to help your nervous system metabolize adrenaline.
In those cases, too, they aren't going to cause digestive distress. It's very bioavailable. It's able to support your system. You're pointing to getting your test results so you know where you might have some specific insufficiencies. I appreciate everything that you've shared with us. I've learned a lot. I intend to finish your book and perhaps even share some of it on the show as a quote here and there because there are some pearls of wisdom that are very helpful to hear again, even that key thing of trying to get a little bit of protein in each snack or meal and searching out those things that make you feel good when you consume them as opposed to those that make you feel laid and down. Are there any closing thoughts that you would like to share?
Thank you so much for this conversation. I love that you found so many good snippets of wisdom in the book. It was a joy for me to be able to write it and share about it. I do also include in the book about spirituality. If people are interested in that level, too and even psychedelic medicine, I'm willing to say, "What do we need as humans? What can we learn from nature and our experience that can help us reset from stress?" That's what I would say. Use this as a tool to help you be inspired. I love that you are already doing that, Corinna.
It's nice to see so much common sense peppered in with all the research too. The thing I would say to everybody here is to try to listen to your body. Sometimes that's, "How did I feel when I woke up in the morning?" Journaling about it can be an incredibly useful tool as well. Thank you so much for joining me.
You're welcome.
---
I also encourage you to reach out and follow her on social channels. She is @DrDoniWilson on Instagram. If you have specific questions about what we covered or topics that you would like us to dive into more, please reach out via our social channels @OrloNutrition, or you can send me an email directly to Hello@OrloNutrition.com. As we close this show, I hope that you will raise a cup of your favorite beverage with me, perhaps it's water or coffee, as I'm drinking and as I say my closing words. Here's to your health.
Important Links
- Master Your Stress, Reset Your Health
- DoctorDoni.com
- The Real Truth About Hormonal Balance with Dr. Shawn Tassone, America's Holistic Gynecologist
- Become a Nutritarian to Supercharge Your Immune System and Health with Joel Fuhrman, MD, the 7X New York Times Bestselling Author of Super Immunity and Eat for Life
- The Emerging Research World of Omega-3 Absorption for Brain Health with Professor Melanie Plourde, Université de Sherbrooke, Québec, Canada
- @DrDoniWilson - Instagram
- @OrloNutrition - Instagram
- Hello@OrloNutrition.com
About Doni Wilson, ND

DR. DONI WILSON is a Naturopathic Doctor, certified professional midwife, certified nutrition specialist, and bestselling author of Master Your Stress, Reset Your Health. For more than 22 years, she has helped thousands of patients overcome health challenges and achieve wellness by using specific strategies that address the whole body and ultimately resolve the underlying causes of distress. Dr. Doni suffered from migraines for over 20 years, and in the process of solving them, she developed her Stress Recovery Protocol. Dr. Doni brings awareness to the impact of stress on our health and how it is possible to recover from burnout and become resilient to stress in the media and at public and professional events. You can find her blog, podcast, called How Humans Heal, and her Self C.A.R.E.TM program at DoctorDoni.com